Article
As winter approaches for much of the northern hemisphere, is an avian flu pandemic guaranteed to occur?
Learn the why behind the headlines.
Subscribe to the Real Truth for FREE news and analysis.
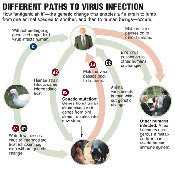
Subscribe NowViruses—they’re super-tiny and super-powerful, and they infect virtually all life, from humans and animals to plants, and even fungi and bacteria. Viruses cause the common cold, influenza and even AIDS (resulting from HIV—the human immunodeficiency virus).
Of particular concern in recent months are the outbreaks in Asia of a virulent form of avian (or bird) flu: a version of the influenza virus that (1) primarily affects birds and (2) spreads quickly, with devastating results.
There are many forms of the influenza virus, each of which primarily affects one type of host. There is swine flu, horse flu, and of course, as mentioned, bird flu. In addition, each form constantly changes slightly (mutates).
This is why there is such great concern about the super-virulent form of bird flu. While some people have contracted it and have died, the expectation and greater fear is that it will change slightly so that transmission and infection from human-to-human would occur, thus resulting in a pandemic, causing great loss of human life. Reports of a pandemic coming this winter exist, while some believe that it may not occur yet, but that it is only a matter of time. Drug companies are increasing production of anti-flu medications, and governments are stockpiling these and scrambling to devise pandemic “battle plans.”
We will consider the basic scientific explanation of how all this is possible; we will take a look at the reasons for current fears and the fallibility of plans and responses; more importantly, we will put the avian flu and a possible influenza pandemic in a realistic, but critical, light.
Understanding Viruses
Viruses are extremely simple organisms that consist only of genetic material surrounded by a protein coat, which is sometimes enclosed in an outer lipid envelope. They are so small (20 to 100 times smaller than the average bacteria) that they cannot be seen by a light microscope. Yet they are not what science considers “free-living,” as they are not able to reproduce by themselves. Viruses must infect a host’s cells to replicate itself.
Upon entering a host’s structure, a virus will “dock” at a specific point on one of the host’s cells (usually a specific type of cell, e.g. HIV binds to the CD4 molecule found on certain human white blood cells). After binding to an appropriate cell, the virus must then penetrate the cell membrane, or “skin,” to enter the host cell. Once inside, it is now free to replicate, often using the host’s cellular machinery. In the matter of a couple hours for small viruses, or up to several days for larger ones, replication is complete, and several new viruses are ready to exit the host cell to infect other cells and continue the vicious cycle of infection and replication. Quite often, as the new viruses exit, the host cell is either damaged or destroyed. The whole process is somewhat like a spy infiltrating an enemy country and then taking over a factory to secretly produce arms that will eventually be used to attack the “host” country.
The human body has been created with several defense mechanisms against viruses. Infected cells produce substances that warn neighboring cells of the problem, thus enabling them to initiate defensive responses. These same substances will often trigger the body to raise its temperature (i.e. a fever), which inhibits the growth of some viruses. In addition, specific defense cells target both viruses themselves and virus-infected cells for inactivation and/or destruction.
However, with the viruses’ ability to mutate, some have been able to circumvent some of these defense mechanisms. This, combined with the poor environment (food, water, air, etc.) in which we live, results in increased infections and outbreaks—and, ultimately, pandemics.
Flu Outbreaks
The flu, caused by the influenza virus, affects the respiratory tract, typically causing coughing, sore throats, runny nose, aches and pains, fever, etc. In severe cases, it is sometimes accompanied or followed by pneumonia.
There have been at least 31 influenza pandemics (widespread epidemics or outbreaks) since the 1500s, the most destructive of which, at least in modern times, was that of 1918. It is estimated to have killed between 20 and 40 million people worldwide, of which 500,000 to 700,000 were in the U.S. Most of the deaths involved cases in which the influenza was followed by the complication of bacterial pneumonia.
In November 2005, The Janesville Gazette published an article detailing the outbreak of the 1918 flu in Janesville, Wisconsin:
• By October 24, 1918, the city health official reported more than 600 flu cases across the city, more than double the number of the week before.
• Victims died painfully, “struggling to clear their airways of a blood-tinged froth that sometimes gushed from their mouth and nose…”
• Public meetings were banned, theatres closed, store hours curtailed; people wore masks in public and infected homes were marked with a red tag.
• Two days later, the number infected reached 708; two days later, at least 769 people were sick. Janesville was averaging 46 new cases a day.
Chronology Of Avian Influenza
• 1890: First recorded recent influenza pandemic.
• 1918: The “Spanish flu” pandemic, caused by H1N1 influenza virus, kills more than 40 million worldwide.
• 1957: The Asian flu pandemic, caused by H2N2 influenza virus, kills 100,000 people.
• 1968: Hong Kong flu pandemic, caused by H3N2 influenza virus, kills 700,000.
• May 21, 1997: For the first time, Avian flu H5N1 is isolated, from an infected human patient in Hong Kong.
• 1999: Tamiflu licensed in U.S., Europe.
• Feb. 2003: Avian flu H5N1 infects two people in Hong Kong, one fatally. On the 28th, outbreaks of the chicken flu, caused by H7N7 avian influenza virus, occur in The Netherlands. By April, 11 million chickens are culled and 83 people are infected, one fatally.
• Dec. 2003: South Korea has its first outbreak of H5N1 avian flu in chickens. Two tigers and two leopards, fed on fresh chicken carcasses, die unexpectedly at a Thailand zoo; subsequent investigation identifies H5N1 in tissue samples.
• Jan. 2004: Japan has its first outbreak of H5N1 avian influenza since 1925; China confirms incidence of H5N1; the World Health Organization (WHO) confirms H5N1 infection in 11 people, eight fatal, in Thailand and Vietnam.
• March 2004: Avian H5N1 influenza virus becomes widespread among Asian bird flocks, including 34 human cases, with 23 deaths.
• April 6, 2004: Avian H7N3 influenza virus confirmed in two poultry workers in British Columbia, Canada.
• July 2004: Despite control efforts, several countries in Asia report new outbreaks in poultry with H5N1.
• Aug. 2004: H5N1 kills another three people in Vietnam; Chinese scientists report H5N1 avian influenza infection in pigs; H5N1 has spread throughout most of SE Asia, resulting in the culling of over 100 million chickens; in Vietnam and Thailand, H5N1 has infected at least 37 people, killing 26.
• Dec. 2004: Since the start of 2004, H5N1 has caused the death of 32 people in Vietnam and Thailand.
• Feb. 2005: 13 new cases (since December) of H5N1 human infection in Vietnam, 12 fatal; a report of probable human-to-human transmission of H5N1 is published in New England Journal of Medicine.
• March 2005: 15 additional cases of H5N1 human infection in Vietnam, and one additional case in Cambodia, are reported.
• April 2005: Vietnam confirms 60 human cases of H5N1 infection, with 35 deaths; Thailand confirms 17 cases, of which 12 have died; Cambodia confirms two fatal cases; wild birds at a lake in central China, where hundreds of thousands of migratory birds congregate, begin to die—in the following weeks, the count reaches over 6,000.
• May 19, 2005: WHO reports 97 cases and 53 deaths from H5N1 avian influenza in Vietnam, Cambodia and Thailand since January 2004.
• June 2005: Avian flu becomes resistant to the low-cost amantadine family of antiviral drugs.
• July 2005: The Philippines and Indonesia report cases of human infection with H5N1.
• Aug. 2005: WHO confirms three new cases of H5N1 in Vietnam; since December 2004, 20 of 63 Vietnamese cases of H5N1 have been fatal; both Russia and Kazakhstan report outbreaks of avian flu, later confirmed as H5N1.
• Oct. 2005: Greece becomes the first EU country with an avian flu infection, confirmed to be of the H5 strain, but not yet identified as H5N1; fifth case in Indonesia brings the total number of human infections with influenza A (H5N1) since December 2003 to 117; H5N1 confirmed in poultry in Turkey and Romania; Croatia confirms H5N1 in wild birds.
• Nov. 2005: H5 confirmed on poultry farm in British Columbia, Canada; Chinese officials say they will vaccinate the country’s entire stock of 14 billion poultry against avian flu.
• Dec. 2005: Ukraine confirms H5N1 in birds on Crimean peninsula; five-year-old Thai boy becomes 70th Asian to die from H5N1.
Source: www.nature.com; the World Health Organization; the Canadian Broadcasting Corporation.
• The citizens read headlines reporting the flu in other places: Merchant Marine sailors stricken in Massachusetts; soldiers dying in East Coast camps; 50,000 sailors quarantined at Great Lakes Naval Base outside Chicago.
• In the end, the official record of deaths in Janesville (a town of 18,200) due to influenza was not found, but it is likely that hundreds died.
The above illustrates quite clearly the speed at which an epidemic travels—and, ultimately, how feeble are mankind’s attempts to stop it.
The three types of influenza virus (known as A, B and C) are what scientists call “antigenically unrelated,” which basically means that being immune to one type does not mean you are immune to the others. This has made preventive treatment extremely difficult. In addition, the influenza virus mutates so rapidly that new vaccines must be developed each year (i.e. typically, the vaccine is based on the most virulent form from the previous year). Viruses regularly mutate largely because they lack the repair systems that cells have. Environmental variables may also play a part in the increased rate of mutations.
Some scientists believe the evidence indicates that the various types of the influenza virus appear in cycles. For example, the variant appearing in the 1978-79 season was identical to the virus that was widespread during the early 1950s. This is one reason why mass inoculation was carried out in the U.S. in the late 1970s. A BBC report indicates that there is an approximate 30-year cycle, which means that we are due for another outbreak.
The Current Avian Flu Crisis
The super-virulent form of avian flu that is currently in the news has been identified as a strain of H5N1 (a form of influenza A); it originally emerged in 1997. Outbreaks of this flu have caused the death or culling of tens of millions of birds. More than 100 people have been infected by this flu, with a mortality rate of 50%. This form has been the focus of much concern amid warnings that the H5N1 could mutate into a form that causes a global pandemic with a high mortality rate.
In early 2005, The New Yorker reported that the vicious avian flu was on the verge of becoming an epidemic. Scott Dowell, the director of the International Emerging Infection’s Program in Thailand, commented, “The world just has no idea what it’s going to see if this thing comes. When really. It’s when [sic]. I don’t think we can afford the luxury of the word ‘if’ anymore…The clock is ticking. We just don’t know what time it is.”
Robert Webster, a virologist who has been studying avian influenza for decades, is even starker: “This is the worst flu virus I have ever seen or worked with or read about.” He also said, “We have to prepare as if we were going to war…the virus is a very promiscuous and effective killer.”
By late summer 2005, a report in The Times (London) of avian flu on the eastern side of the Ural Mountains (separating Europe from Asia) had raised concern, although the outbreak was not yet confirmed to be the deadly H5N1 strain. Roads were cordoned off in parts of Siberia, as hundreds of chickens were slaughtered in an attempt to control the spread of the virus.
Gennadi Onishchenko, Russia’s top state epidemiologist, predicted that the virus would soon spread to Russia’s agriculture regions of Krasnodar, Stavropol and Rostov in the south, and then on to the Middle East and the Mediterranean: “An analysis of bird migration routes has shown that in autumn 2005 the H5N1 virus may be spread from Western Siberia to the Caspian Sea and the Black Sea. Apart from Russia’s south, migrating birds may spread the virus to nearby countries (Azerbaijan, Iran, Iraq, Georgia, Ukraine, and Mediterranean countries) because bird migration routes from Siberia also go through those regions in autumn.”
Dr. David Nabarro, of the World Health Organization, said, “We expect the next influenza pandemic to come at any time now…” and could result in as many as 150 million deaths worldwide. Even the lowest expected death toll is 5 million, said Dr. Nabarro, as he called upon governments to take immediate steps: “The work we’re doing over the next few months on prevention and preparedness will make the difference between, for example, whether the next pandemic leads us in the direction of 150 [million] or in the direction of 5 [million]” (Associated Press).
Chilling words!
In addition to the loss of human lives, there is also the toll that a pandemic would take on the world economy. The Asian Development Bank (ADB) released a report last week projecting that an avian flu outbreak in Asia could kill approximately three million people, cost $300 billion and push the world into a recession. However, the report assumed a 0.5% mortality rate, whereas current cases of H5N1 are at 50%!
Man’s Attempts to Protect Himself
Historically, mankind’s attempts to protect himself have revolved, rightfully so, around cleanliness and sanitation. Rodent control, food processing and storage, sewage systems and clean water have accomplished much in the last century to control disease. And yet, in general, these luxurious advances are commonplace only in the Western world. Outbreaks of SARS and avian flu are originating in parts of the world where sanitation is minimal.
The Avian Influenza A Virus
Avian influenza A H5 and H7 viruses can be distinguished as “low pathogenic” and “high pathogenic” forms on the basis of genetic features of the virus and the severity of the illness they cause in poultry; influenza H9 virus has been identified only in a “low pathogenicity” form. Each of these three avian influenza A viruses (H5, H7, and H9) theoretically can be partnered with any one of nine neuraminidase surface proteins; thus, there are potentially nine different forms of each subtype (e.g., H5N1, H5N2, H5N3, H5N9).
Summary information about these three prominent subtypes of avian influenza A viruses follows:
• Influenza A H5 – Potentially nine different subtypes; can be highly pathogenic or low pathogenic; H5 infections have been documented among humans, sometimes causing severe illness and death.
• Influenza A H7 – Potentially nine different subtypes; can be highly pathogenic or low pathogenic; H7 infection in humans is rare, but can occur among persons who have direct contact with infected birds; symptoms may include conjunctivitis and/or upper respiratory symptoms.
• Influenza A H9 – Potentially nine different subtypes; documented only in low pathogenic form; at least three H9 infections in humans have been confirmed.
Source: U.S. Centers for Disease Control and Prevention
In 1796, British physician Edward Jenner observed that milkmaids in England who contracted the mild cowpox virus infection from their cows were protected from smallpox. Similar viruses cause both cowpox and smallpox. By 1798, Jenner formally demonstrated that previous cowpox infections protected that person from smallpox. This was the beginning of the vaccine, which is simply a concoction prepared from killed or weakened viruses, or sometimes even just pieces of a virus. Each of these, upon injection, will elicit the immune response, while causing little or no disease. Of course, the modern application of vaccines, considering mass production with questionable, oftentimes harmful, ingredients, is of some concern.
The primary difficulty in developing antiviral medicines is that, as we have seen in regard to influenza, a large number of variant viruses can cause the same disease. In addition, it is extremely difficult to create a drug that attacks a virus-infected host cell without disabling healthy cells.
Vaccines are increasingly popular and recommended by health officials, governments, etc. At one time, only those at risk of contracting pneumonia were administered annual flu shots. But in 1984, the U.S. Centers for Disease Control recommended that medical personnel, as well as anyone who desired it, be added to that list.
At the moment, the world is investing a lot of money in a drug called Tamiflu, produced by Swiss drug giant Roche. Pharmaceutical companies make a lot of money from drugs that are in high demand; with demand for Tamiflu outstripping supply, Roche has been hesitant to sign sublicensing agreements. In fact, in December 2005, the International Herald Tribune reported that Roche had signed its first sublicense contract with China’s state-owned Shanghai Pharmaceutical Group. Talks with 12 other companies continue. According to the article, Tamiflu has been found in clinical trials to work against the symptoms of the H5N1 strain of influenza. Note, however, that working against the symptoms has little to do with controlling the spread of the virus.
Ultimately, if we take the 1918 epidemic as an example, or almost any disaster for that matter, man’s ability to protect himself has been largely unsuccessful. There are reasons for this.
What God Says
Man is nearing the end of a 6,000-year period during which his Creator, God, allowed him to live life his own way. Though this has brought some relatively minor accomplishments, it has also produced widespread heartache, misery, suffering and destruction.
There was a time when modern medicine thought it could control disease. Bold initiatives were formulated and implemented to eradicate smallpox and polio, yet only with limited success. In addition, old diseases such as tuberculosis are once again rearing their ugly heads, but this time in antibiotic-resistant forms.
There is a law of cause and effect. When laws are broken, penalties must be paid, either immediately or after a long period of time. God has warned mankind—who has cut himself off from his Creator (Isa. 59:2)—that diseases would come to those who do not obey Him. In addition, several scriptures (Matt. 24:7, Rev. 6:7-8) point to a time near the end of that 6,000-year period when “pestilences” would increase. Ezekiel 5:12 reveals that, during end-time events, one-third of the population of the modern-day descendants of Israel will die by diseases.
With wild birds migrating across the world, spreading the H5N1 virus amongst themselves, and then to domestic flocks, the number of infections will increase globally. And with this will come a greater chance for a mutation that will render the virus transmissible from human to human.
We do know that disease outbreaks are certain to increase.


